Obesity and inflammation: genetic predisposition and therapy

Obesity is often accompanied by a heavy social stigma, reducing this complex condition to a matter of willpower or lack of self-control, while ignoring the multiple genetic, metabolic, and environmental factors that profoundly influence it.
While often not perceived as such, obesity is a genuine chronic disease, and the excessive accumulation of body fat it entails poses significant health risks. Obesity is indeed associated with a series of metabolic complications not to be underestimated, such as cardiovascular diseases, fatty liver, dyslipidemia—meaning excessively high cholesterol and triglyceride levels—insulin resistance, and diabetes.
Causes of obesity
The causes of obesity are multiple and interconnected, with the environment and lifestyle playing a significant role in its development.
While obesity was once thought to be simply linked to overeating, such as excessive consumption of junk food, we now know that a low-grade inflammatory condition, coupled with an imbalanced diet, plays a fundamental role in the development of this condition.
Often overlooked is the need to control not only the balance of macronutrients but also the inflammation resulting from repetitive eating patterns and excessive sugar intake, which compromises the ability to lose weight and promotes fat accumulation.
Low-grade inflammation and obesity
In the presence of inflammatory processes, certain cytokines are released, including BAFF (B-Cell Activating Factor). This molecule, by altering sugar metabolism and promoting insulin resistance, favors the accumulation of visceral fat. A high level of visceral fat, in turn, causes chronic inflammation and increased production of BAFF. This sets off a vicious cycle that promotes weight gain and can lead to obesity.
It often happens in clinical practice that patients with an overall balanced diet still notice an increase in fat mass and a decrease in metabolism. This occurs because BAFF production is correlated with the repeated consumption of specific food groups. In such cases, it is necessary to identify these groups and rebalance their intake within the context of a rotation diet, which brings inflammation levels under control.
Another inflammatory molecule capable of promoting insulin resistance is Methylglyoxal, or MGO.
MGO is one of the most potent free radicals. It is produced in harmful quantities when we have a diet rich in simple sugars (found in juices, ice cream, snacks) and substantial amounts of complex carbohydrates (bread, pasta), especially if consumed in unbalanced meals that do not respect the balance between proteins, good fats, and fibers. Alcohol intake also leads to an increase in MGO.
The combined action of MGO and BAFF leads to a worsening of the overweight condition, which can lead to obesity.
Often, people who want to lose weight start replacing sugars (the classic sucrose) with low-calorie or “zero” calorie sweeteners, such as sorbitol, mannitol, erythritol, unaware that these substances still promote the production of MGO, with the final effect of raising the body’s inflammation level and hindering weight loss.
Genetic predisposition to obesity
Recent studies highlight how the presence of a specific genetic variant (SNP) in the FTO gene is associated with the development of obesity. The risk, for those with this variant, of developing obesity and overweight is 1.4 times higher than the population without this predisposition.
This genetic variant does not guarantee the development of the disease, and epigenetic components (environment, lifestyle) prevail. However, knowing one’s predisposition helps understand if there is a structural, genetic aspect that facilitates weight gain and allows for the implementation of dietary and integrative strategies in a preventive manner.
Therapeutic approaches to obesity
To restore a healthy and balanced diet, it’s essential to start with the Harvard Healthy Plate, which ensures a proper intake of protein, carbohydrates, and plant-based fibers for each meal. This approach helps to regulate insulin secretion and prolong the feeling of satiety, preventing the need for snacks and mid-meal nibbles, which is a common issue for those dealing with obesity.
Additionally, promoting muscle growth (and thus calorie consumption and weight loss) is achieved by distributing the protein intake across all three meals of the day, including breakfast. We have dedicated a detailed article to compare diets, and we encourage you to read it.
Often overlooked is the need to control not only the balance of macronutrients but also the inflammation resulting from repetitive eating patterns and excessive sugar intake, which compromises the ability to lose weight and promotes fat accumulation.
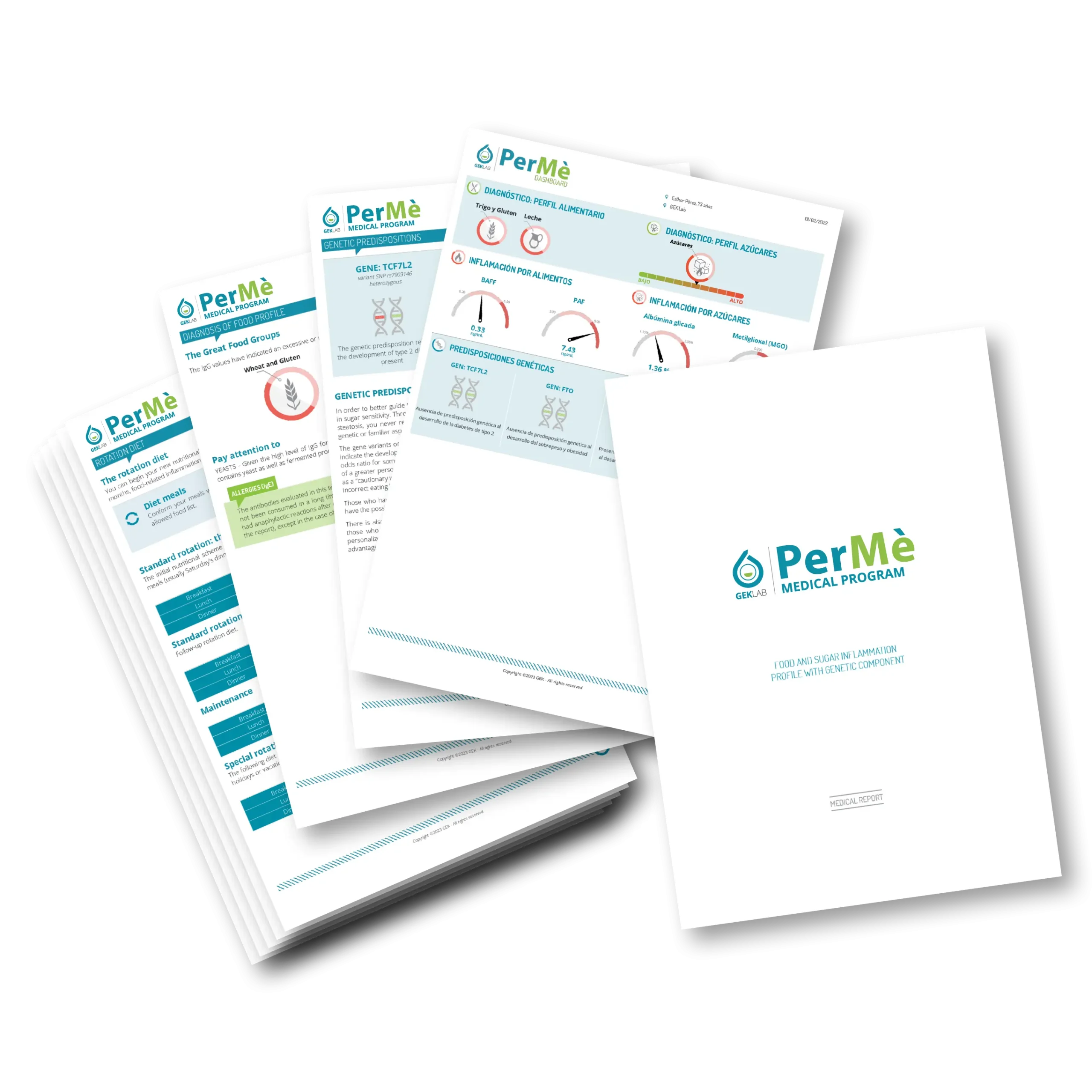
By undergoing the PerMè Medical Program (which evaluates both inflammation from sugars and from foods), it’s possible to identify which food groups are causing inflammation and therefore the root cause of weight loss difficulty. Knowing your exact dietary profile is the starting point for setting up a personalized rotation diet, based on the indications provided in the report, which is sustainable and yields tangible results.
PerMè also assesses the presence of genetic variants such as SNP and other genetic polymorphisms that characterize a higher personal susceptibility to developing diabetes, fatty liver disease, and autoimmune diseases.
To bring weight gain under control, it’s also necessary to restore the right balance between fat mass and muscle mass. In this regard, physical activity should be approached as a true therapy. It’s important to engage in cardio workouts (such as running, brisk walking, or cycling) because they improve glycemic control, blood pressure, and cardiovascular health.
However, strength training exercises are also important: increasing muscle mass raises metabolism and leads to an improvement in glycemic sensitivity. Muscle has the ability to modulate blood sugar levels by opening channels on the cell membrane (called GLUT 4). Therefore, the amount of muscle is directly proportional to the ability to uptake circulating sugars, avoiding glycemic spikes and insulin resistance.
In some cases, supplements may be prescribed (such as chromium, a natural hypoglycemic, and inositol, which acts on insulin resistance), but also medications to aid in weight loss or manage comorbidities associated with obesity.
In cases of severe or treatment-resistant obesity, surgical intervention may be considered.
Conclusions
Obesity is a complex condition that requires an integrated approach involving lifestyle changes and psychological support. Low-grade inflammation plays a significant role in the development and complications of obesity, and it’s important not to overlook this aspect in managing the condition.
By the Scientific Editorial Team at GEK Lab