Managing asthma and seasonal respiratory allergies

The arrival of the spring season brings bright days and milder temperatures. However, for some of us, spring brings along another less pleasant aspect: asthma and seasonal respiratory allergies.
In this article, we will explore these conditions and share some strategies to successfully manage them.
What is asthma and why does it occur?
Asthma is a condition of the respiratory tract characterized by inflammation and narrowing of the bronchioles. This leads to symptoms such as wheezing, coughing, difficulty breathing and chest tightness.
The onset of asthma symptoms is significantly influenced by a combination of inflammatory, environmental, genetic, and psychological factors.
It also happens that people who once knew they had symptoms from grass suddenly find themselves experiencing symptoms for ragweed or wall pellitory. Often, they have multiple reactions to skin prick tests, or even more strangely, they test negative. All of this necessitates a broader reflection on the subject.
Seasonal respiratory allergies
Seasonal respiratory allergies, such as widespread allergic rhinoconjunctivitis, are allergic reactions to plant, grass, or tree pollens.
When exposed to these substances, our immune system may react inconsistently, triggering a series of unpleasant symptoms such as sneezing, itchy eyes, tearing, burning of the mucous membranes, runny nose, and, in some cases, worsening of asthma.
Typically, seasonal respiratory allergies were diagnosed in childhood, followed by a decrease in symptoms over the years. Epidemiological data tell us that, contrary to the past, an increasing number of people start sneezing at twenty or fifty years old, with symptoms indistinguishable from the classic ones of allergies or allergic asthma. Certainly, climate change is leading to diversified blooms, and old seasonal patterns are strongly modified.
It also happens that people who once knew they had symptoms from grass suddenly find themselves experiencing symptoms for ragweed or wall pellitory. Often, they have multiple reactions to skin prick tests , or even more strangely, they test negative. All of this necessitates a broader reflection on the subject.
Similar allergic symptoms and the role of sugars
Since 2017, it has been documented that only 38% of cases of similar allergic reactions can be attributed classically to an “allergic” cause, meaning the immune system response to pollen, food, or medications. In the remaining 62% of cases, reactions are often multifactorial in nature and are frequently correlated with glycation, or the effect of sugars (and metabolically related substances such as alcohol and polyols) taken in excess.
An important scientific study, published in 2023 in Frontiers in Allergy, finally explains in detail the biochemical and molecular mechanisms that cause the inflammatory reaction, with effects entirely similar to allergic ones, caused precisely by glycating substances, of which we remember that the prototype is Methylglyoxal.
Glycating substances raise the body’s alarm level, altering the physiological functioning of the immune system, and causing antigens, i.e., allergenic substances of any kind, to be perceived differently than usual. In other words, individually excessive sugar consumption causes the body to begin to consider pollen or external agents (such as dust or mites) that until recently encountered our respiratory system without causing problems, as “enemies.”
Further confirmation of the relationship between diet and allergic or inflammatory response was provided by an article published in JACI in September 2021, in which important researchers from the Universities of Pittsburgh and Rochester (USA) explained that it is very likely that the combined effect of diet contributes to the onset of asthma. This implies that focusing exclusively on a specific antigen or IgE may be ineffective. It is important to consider factors such as the inflammatory potential of the diet, the intake of antioxidants, and the energy regulation of foods together.
How to deal with asthma and respiratory allergies
Given that investigating respiratory allergens is a procedure that continues to hold diagnostic and therapeutic value, and that the use of antihistamines may sometimes be necessary, successfully treating asthma requires considering all other conditions that may contribute to or cause respiratory difficulties.
Since, as we have explained, there is a concrete possibility that a condition of inflammation from sugars or foods may underlie the symptoms, it is always advisable to investigate the levels of such inflammation. In other words, it happens that even asthma, watery eyes, and incessant runny noses may need, to heal, to modulate dietary habits that generate inflammation.
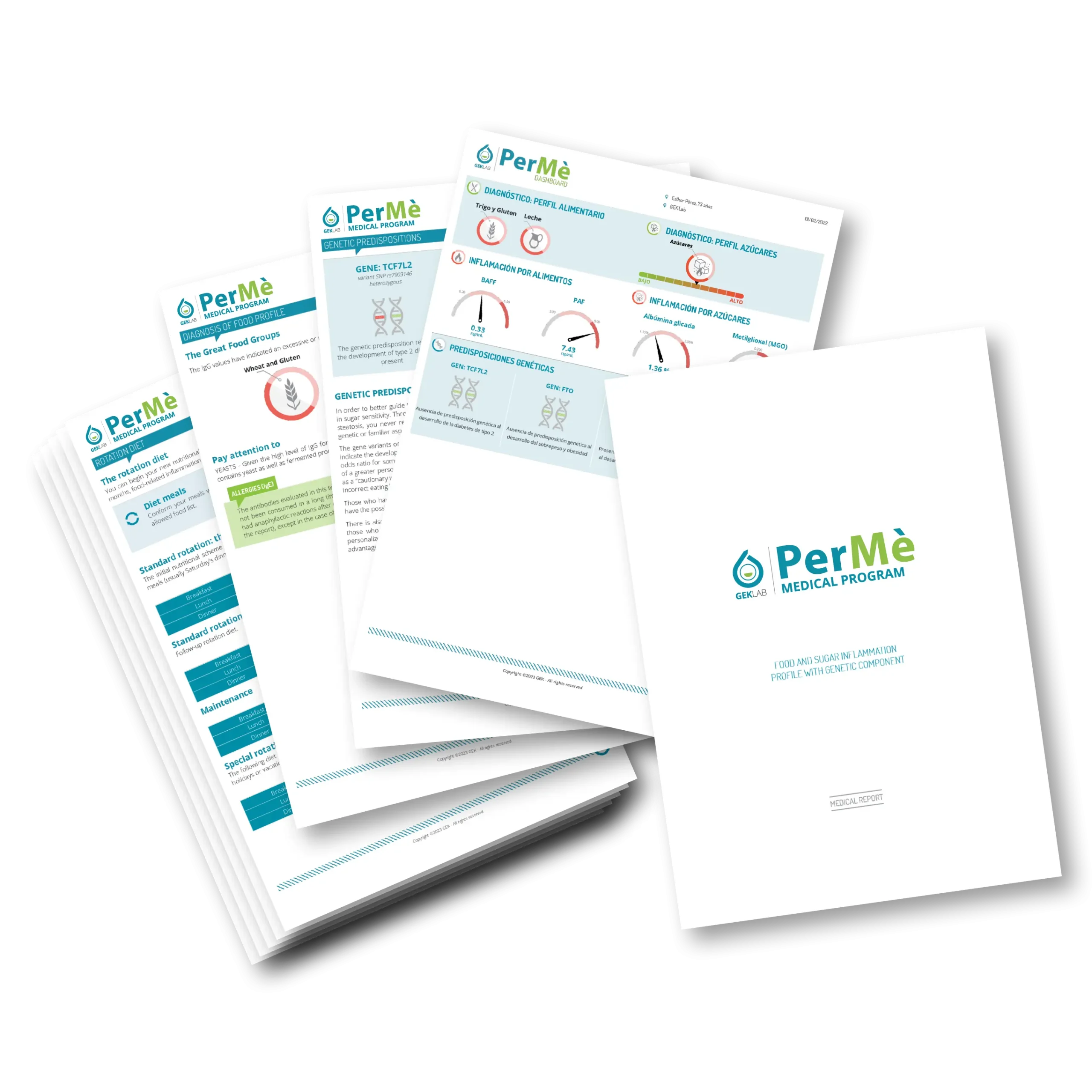
By performing a PerMè Medical Program, it is possible to measure one’s level of glycation (by detecting Methylglyoxal and Glycated Albumin) and inflammation from excessive consumption of certain classes of foods (by detecting BAFF and PAF).
The medical report accompanying the report results will allow for the implementation of a personalized diet that, by controlling sugar and food intake, reduces inflammation and addresses similar allergic symptoms, sometimes resolving them completely.
By the Scientific Editorial Team at GEK Lab
No post found!