Infertility is an emotional and medical challenge that affects millions of individuals worldwide. While the causes can be varied and complex, one of the most promising research avenues in recent years has focused on inflammation and its impact on both male and female fertility. In this article, we will explore the link between infertility and inflammation, providing an overview of the scientific basis behind this relationship and the implications for diagnosis and treatment.
Male infertility and inflammation
Male infertility is often associated with disorders of sperm production, quality, and/or motility. Recently, research has shown that inflammation can play a crucial role in many of these situations. Inflammation at the testicular or epididymal level can damage the spermatic tubules, interfere with sperm production, and compromise its functionality.
Recognizing the role of inflammation in infertility is crucial for guiding effective diagnostic and therapeutic strategies. Therapeutic approaches that aim to reduce inflammation can indeed improve both male and female fertility.
Inflammation can compromise reproductive capacity through various mechanisms, including the inhibition of absorption of specific nutrients essential for spermatogenesis, and the production of free radicals (ROS) (directly linked to the presence of glycation products and AGEs) or inflammatory cytokines (such as BAFF, PAF, TNF-alpha, and Interleukin-6), which significantly alter the microenvironment where sperm development and maturation occur. Elevated levels of inflammatory cytokines and the production of free radicals in the epididymis and testicles can damage sperm DNA and reduce overall quality.
Systemic inflammation, including that induced or sustained by nutrition and sugars, along with an unbalanced lifestyle, can play a fundamental role in testicular dysfunction.
Female infertility and inflammation
Similarly, inflammation significantly impacts female fertility by influencing ovarian function. Conditions such as endometriosis, chronic pelvic inflammation, and upper genital tract infections can compromise ovarian function, ovulation, and uterine health.
Chronic inflammation can also interfere with embryo implantation in the uterus, thereby reducing the chances of pregnancy continuation and increasing the risk of miscarriage.
Inflammation can also hinder the function of the fallopian tubes, preventing the passage of eggs to the uterus and their encounter with sperm, a crucial process for conception.
For all these reasons, controlling inflammation (including through personalized nutritional changes) is a key element in supporting assisted reproductive technology (ART) procedures.
What to do
Recognizing the role of inflammation in infertility is crucial for guiding effective diagnostic and therapeutic strategies. Therapeutic approaches aimed at reducing inflammation can indeed improve both male and female fertility.
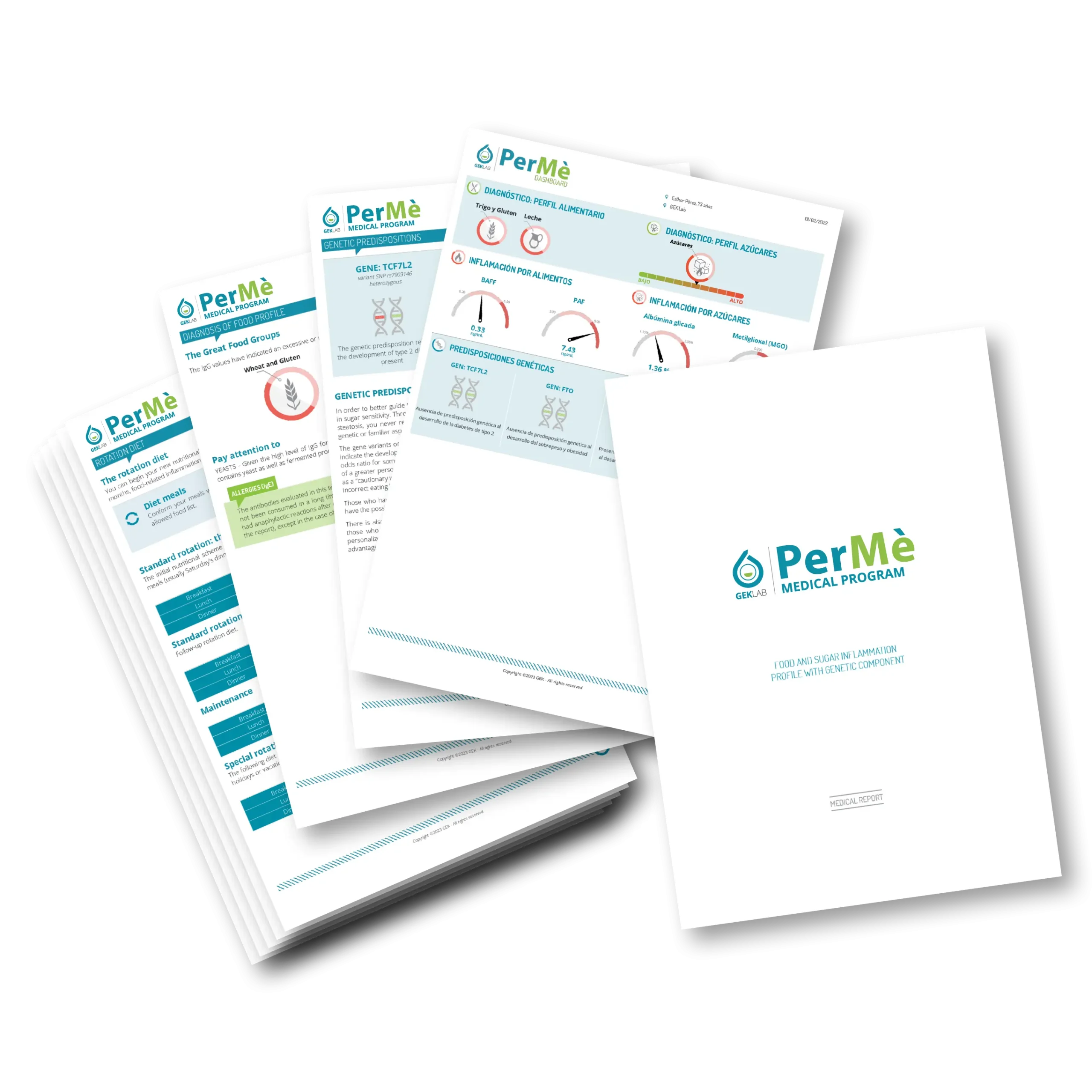
Reading inflammation levels, easily measurable by the PerMè Medical Program, allows for the development of a personalized anti-inflammatory diet. This diet effectively reduces systemic inflammation and, consequently, improves the environment in which male and female germ cells develop.
The personalized dietary profile provided by the report suggests a highly customized diet plan that reduces the interference of inflammatory and glycating substances in the production and maturation of eggs and sperm, facilitating the implantation of the fertilized egg while controlling systemic inflammation.
This personalized anti-inflammatory nutritional therapy is also useful in all situations of subfertility (such as polycystic ovary syndrome or oligospermia) or in supporting assisted reproductive technology (ART) procedures.
Other conditions to keep under control
Overweight and obesity: visceral fat is associated with increased insulin resistance and chronic inflammation, and its excess can exacerbate fertility-related issues. Maintaining a proper body composition through diet and an active lifestyle is of paramount importance. In men, obesity can lead to increased estrogen production, which negatively influences sperm production and vitality.
Resistenza insulinica: il consumo eccessivo di zuccheri, alcol e polioli (i comuni dolcificanti) e altre condizioni endocrine (come l’ovaio policistico) possono favorire resistenza insulinica, una condizione in cui le cellule del corpo diventano meno sensibili all’insulina, l’ormone prodotto dal pancreas che regola i livelli di zucchero nel sangue. La resistenza insulinica contribuisce all’accumulo di adipe in sede viscerale, a un aumento della produzione di androgeni e può compromettere l’ovulazione e influenzare negativamente la qualità degli ovuli e dello sperma.
Insulin resistance: excessive consumption of sugars, alcohol, and polyols (common sweeteners) and other endocrine conditions (such as polycystic ovary syndrome) can promote insulin resistance, a condition in which the body’s cells become less sensitive to insulin, the hormone produced by the pancreas that regulates blood sugar levels. Insulin resistance contributes to the accumulation of fat in visceral areas, an increase in androgen production, and can compromise ovulation and negatively affect the quality of eggs and sperm.
Polycystic Ovary Syndrome (PCOS): PCOS is one of the most common endocrine conditions, affecting 13% of women of childbearing age. In patients with PCOS, chronic inflammation can contribute to ovarian dysfunction, excessive production of male hormones, and again, insulin resistance. This inflammatory state can compromise ovulation and hinder fertility. In the case of PCOS, it is important to manage inflammation through diet and physical activity.
Sedentary lifestyle: sedentary behavior can negatively impact fertility, especially in males. A sedentary lifestyle and low muscle tone can alter hormonal profiles (and thus testosterone levels), as well as metabolic profiles. Moreover, prolonged sitting increases scrotal temperature and alters the production and motility of sperm, which are formed inside the testicles.
Conclusions
Infertility is a complex challenge that requires a multifactorial approach. Inflammation is increasingly recognized as a significant factor common to most forms of male and female infertility. Measuring inflammation levels from foods and sugars with the PerMè Medical Program and taking personalized action to reduce them is crucial for improving conception chances and reproductive well-being. Integrating inflammation management through lifestyle changes and, if appropriate, supplements, can be a significant step towards achieving the desired pregnancy.
By the Scientific Editorial Team at GEK Lab
No post found!