Cardiovascular diseases: the role of low-grade inflammation

The term “low-grade inflammation” may sound somewhat reassuring, but it’s actually a key concept that can significantly impact the health of our hearts in surprising ways.
In this article, we’ll explore the link between low-grade inflammation and cardiovascular diseases, seeking to understand how these processes influence the well-being of our cardiovascular system.
What is low-grade inflammation?
Inflammation is a natural response of our body to injuries, trauma, or infections.
Typically, this response is temporary: inflammatory chemicals are released to attract immune system cells to eliminate the harmful agent and repair tissues.
The causes of low-grade inflammation are not isolated but often interconnected. For instance, an unbalanced diet can lead to metabolic dysfunctions (such as obesity, type 2 diabetes), stress, and imbalances in the microbiota, all contributing to chronic inflammation.
However, low-grade inflammation is different: it’s a long-term response that can persist for weeks, months, or even years. It can be caused by factors such as unhealthy lifestyles, persistent infections, imbalances in gut bacterial flora, stress, immune system dysfunctions, repetitive eating patterns, and excessive glycation. These causes are not isolated but often interconnected. For example, an unbalanced diet can lead to metabolic dysfunctions (such as obesity or type 2 diabetes), stress, and imbalances in the microbiota, contributing to chronic inflammation. It’s a more subtle and insidious form of inflammation that can develop at the cellular level without obvious symptoms.
Low-grade inflammation plays a crucial role in the development of cardiovascular diseases: let’s see how.
Formation of atherosclerotic plaques
In conditions of inflammation, the endothelial cells lining the walls of arteries can become more permeable and “welcoming” to lipoproteins, especially low-density lipoproteins (LDL), commonly known as “bad cholesterol.” The accumulation of LDL in the artery walls is the first step toward plaque formation.
Subsequently, immune system cells also accumulate in inflamed areas. This process can lead to the formation of deposits that make arterial walls thicker and less elastic. Over time, plaques can grow, partially or completely obstructing blood flow.
Heart attack and stroke
Atherosclerotic plaques can become unstable and prone to rupture over time. When a plaque ruptures, it can cause the formation of a blood clot on the damaged surface. This clot can completely block a coronary artery, leading to a heart attack, or travel through the vascular system to the brain, causing a stroke. In this case as well, inflammation plays a key role in plaque destabilization, through various mechanisms (mainly by degrading some structural components of the plaque, such as collagen).
Arrhythmias, tachycardia, and palpitations
Recent research has allowed the correlation of cardiac arrhythmias (whether it be palpitations, atrial fibrillation, tachyarrhythmias, or extrasystoles) with inflammatory cytokines such as TNF-alpha, BAFF, IL6, and others.
These effects go beyond the direct stimuli exerted by certain foods or beverages, such as caffeine or alcohol.
Some phenomena of cardiac rhythm disturbance, not caused by electrical or anatomical abnormalities of the heart, may instead depend on an induced inflammatory stimulus at the intestinal level, triggered by food intake.
This means that persistent arrhythmia, in the absence of specific alterations in heart muscle, could result from daily and repeated consumption of bread or any other common food.
Assessing the level of inflammation and understanding an individual’s dietary profile can contribute (through an appropriate diet) to the healing process or improvement of such conditions.
Role of sugars and related substances
Excessive consumption of sugars and related substances (including excessive fruit intake, carbohydrate-heavy meals, as well as alcohol and sweeteners) can lead to an increase in various free radicals, including Methylglyoxal. When this substance binds to “good” cholesterol, it causes a decrease in its levels, resulting in an increase in “bad” cholesterol and an elevation in cardiovascular risk. Methylglyoxal also has a high inflammatory potential and generates oxidative stress in cells, including those of cardiac and vascular tissues.
Individually excessive sugar consumption can also cause insulin resistance, which, in addition to being associated with increased inflammation, can contribute to the development of type 2 diabetes.
Systemic inflammation associated with diabetes can also damage arterial walls, contributing to plaque formation and occlusions, following the mechanisms we have already explained. High blood sugar levels also cause stiffness in the blood vessels and affect their ability to regulate blood flow, increasing the risk of hypertension.
Similar to its effect on muscles (as athletes are well aware), Methylglyoxal reduces energy production from mitochondria, and when considering the reduced strength of the heart, one might think of heart failure or circulatory insufficiency. A properly tailored diet can always improve heart function.
Measuring inflammation and preventing cardiovascular diseases
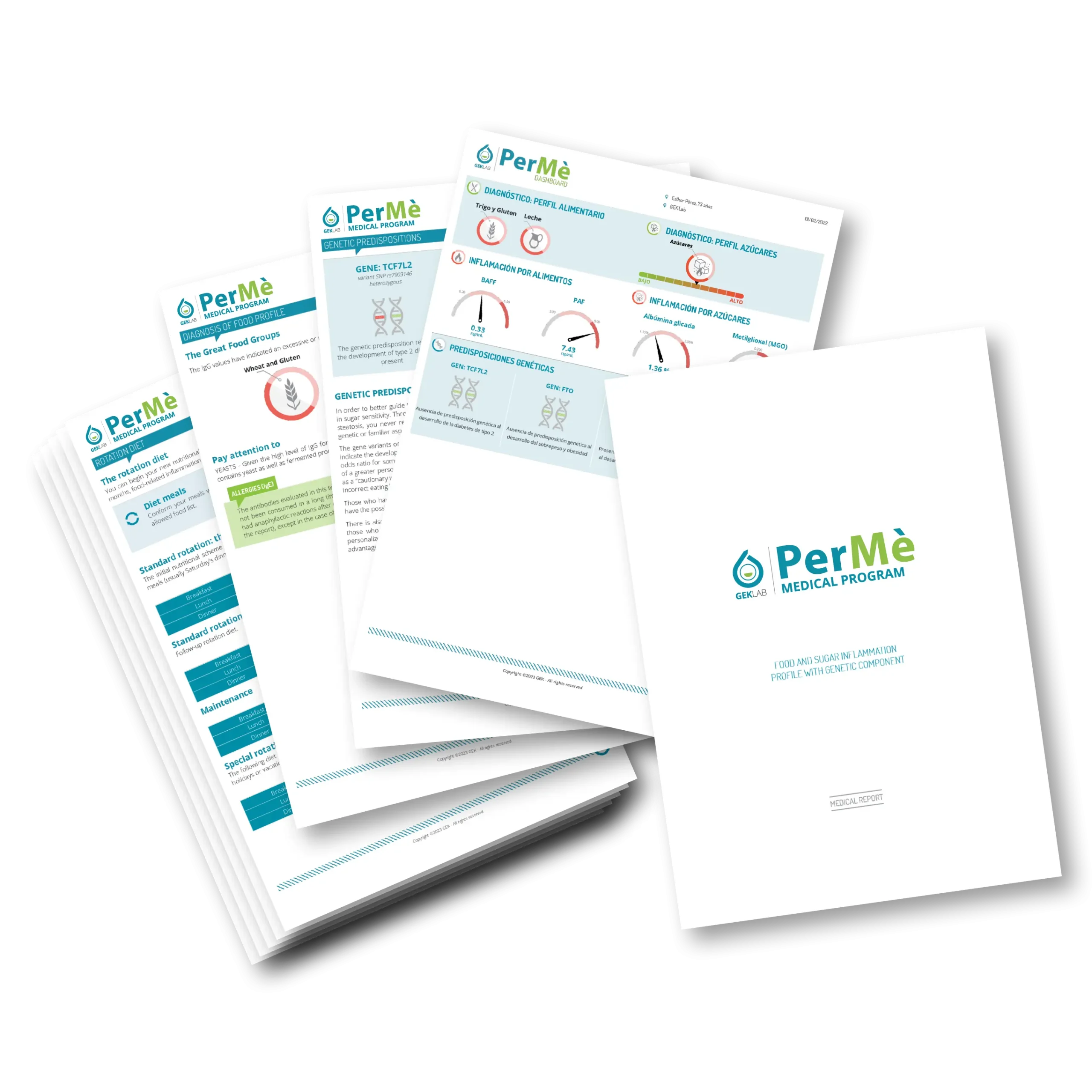
Considering all that has been explained so far, understanding one’s inflammation levels increasingly gains value from the perspective of preventing cardiovascular diseases. Conducting a PerMè Medical Program allows for the measurement of both inflammatory cytokines such as BAFF and PAF, as well as highly sophisticated indicators of sugar-related inflammation such as Methylglyoxal and Glycated Albumin, which also provide valuable information on the likelihood of developing type 2 diabetes.
Measuring these substances and following the advice provided in the PerMè Medical Program allows for the immediate implementation of personalized nutritional choices that help maintain one’s well-being and cardiovascular health.
By controlling inflammation, reducing fat mass, and managing glycemic variability, the foundation is laid for staying healthy and fit in the long term.
By the Scientific Editorial Team at GEK Lab